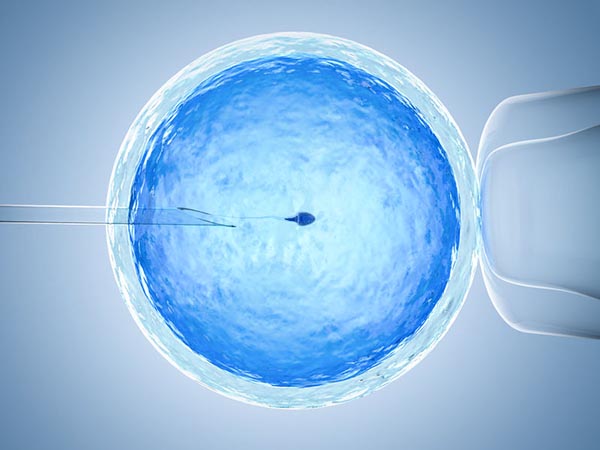
ICSI con espermatozoides morfológicamente seleccionados
Una de las técnicas más novedosas en el mundo de la fertilidad humana es el IMSI, o microinyección de espermatozoides morfológicamente seleccionados.
¿Qué es el IMSI?
Este examen es conocido con las siglas inglesas MSOME (Motile Sperm Organelle Morphology Examination). La micro-inyección oocitaria de espermatozoides seleccionados con este sistema óptico de altísima resolución se conoce como IMSI.
¿Cuál es el alcance de este tratamiento?
El IMSI permite inyectar los oocitos solo con espermatozoides seleccionados de acuerdo a estrictos criterios morfológicos en los que se tiene en cuenta el tamaño y forma de la cabeza y pieza media del espermatozoide y la presencia de vacuolas en la cabeza.
Se ha establecido una correlación entre la presencia de vacuolas grandes en la cabeza de los espermatozoides y la fragmentación del ADN. Se cree pues, que el IMSI “deselecciona” espermatozoides con anormalidades fisiológicas asociadas a la fragmentación del DNA. De esta manera, hasta un 68% de espermatozoides “normales” seleccionados para ser inyectados bajo una resoluciónóptica menor, no cumplen con los criterios de selección del IMSI.
Un reciente meta análisis mostró que la utilización del IMSI aumenta en forma significativa el porcentaje de implantación embrionaria (OR 2.72; 95% IC 1.50-4.95) y de embarazo (OR 3.12; 95% IC 1.55-6.26), y reduce el riesgo de aborto (OR 0.42; 95% IC 0.23-0.78) en comparación con el ICSI. Estudios aleatorios también han mostrado que parejas con ciclos fallidos de ICSI asociados a mala calidad espermática logran embarazos a término luego del IMSI.
Si requieres más información sobre este tratamiento, comunícate con nosotros en nuestras líneas de atención.
- Medellín: Tel. +57(4) 268 80 00
- Bogotá: Tel. +57(1) 746 98 69
- Pereira: Tel. +57(6) 340 17 09
- Cartagena: Tel. +57(5) 693 0434